Population Health Initiative: At the core what Revenues look like
Last article we took a high-altitude look at a population health initiative. Today we are looking at how revenues and capabilities acquired within these core revenue lines help build a successful initiative.
These revenue lines are generated from Medicare-allowables but are transferable to other payer models as they all mostly follow traditional Medicare.
Transitional Care Management TCM, not to be confused with Transformational Care is right at the core, as it provides us the best chance to get started not only gathering data but getting those very sick and recently discharged from an inpatient acute care setting back in front of their primary care physicians. This is crucial as we find that many PCP’s are not aware of the inpatient stay and acuity that caused the admission, let alone the changes and or addition made to the patients care plan and medications. This is the first instance that we are able to coordinate medical treatment plans for better management of the patient’s disease. This is done in either a less than a 7 day CPT Code 99496 or a 14 day CPT Code 99495 window from the date of discharge for the patient to be seen by the primary care physician after discharge as a face to face. Revenues range from 130 to 200 dollars.
Chronic Care Management CCM, becomes the second leg of the core data-gathering in order to have a comprehensive population health initiative. This allows for the collection, aggregation, and management of data from across the continuum and converts the same into one care plan that is actionable and can be supervised by the PCP. This is critical when we know that coordination of care provides better outcomes and saves money just as a standalone. Before this, there was no incentive to manage and collect patient information from other continuum providers while collaborating with patient and PCP to look for gaps or improvements in care.
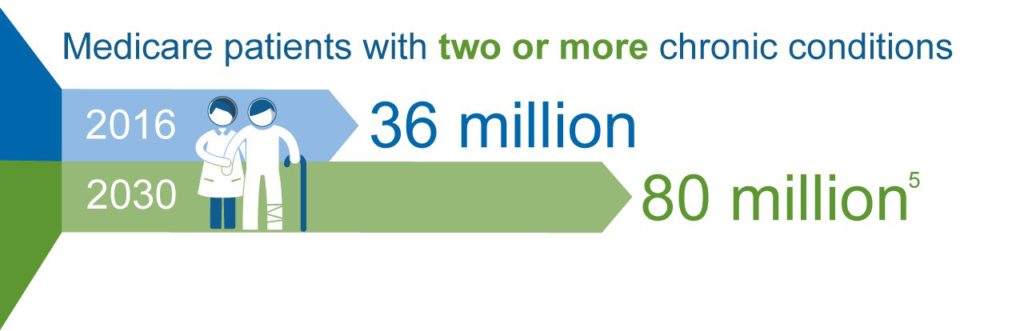
The chronic care management market is big and growing
This started later than TCM, and it is a non-face to face per month per patient amount of monies to manage the care for those that met CMS is chronic care management definition. Key Improvements for 2017: Increased payment and additional codes for 2017, the single CCM code in 2016 paid approximately $42. Now there are 3 codes and payment can range from approximately $43 to over $141, depending on how complex a patient’s needs are. There are requirements by CMS that will have to be in place to bill but the benefits outweigh the requirements.
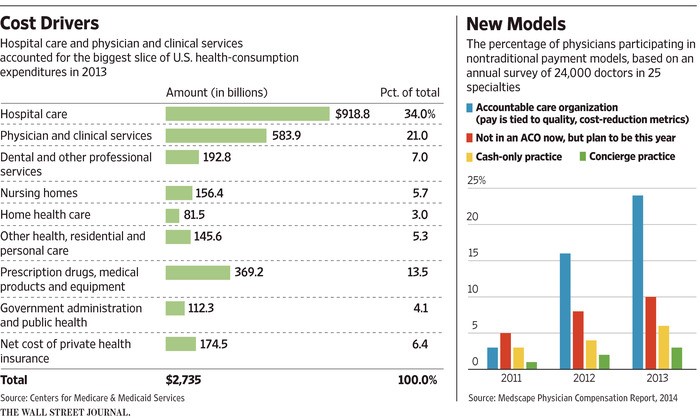
Accountable Care Organizations ACO, these organizations by nature should be using all the tools available to provide “Best Care” while reducing costs. A well thought out initiative should include your PCP’s involved in one of these organizations.
There are many more revenue lines, but these should be at the core of a successful Initiative.

By Mario Espino
Resources for TCM and CCM
Chronic Care Management $50 Billion Market
Moving Ware from Fee for Service








Leave a Reply